Talieh Ghane researches the interaction between light and health at the California Lighting Technology Center. We talked about the biological vs. visual system of light, how to synchronize your circadian clock for better health, healthcare lighting and why you shouldn’t be on your phone right before bed.
As we learn in the interview, healthy lighting strikes the balance between adequate natural lighting, the proper use of LED light color temperature and intensity throughout the day and total darkness.
Language of Light: Can you give an overview of your research on how lighting impacts human biology?
[Ghane’s answers have been paraphrased and edited for clarity and content.]
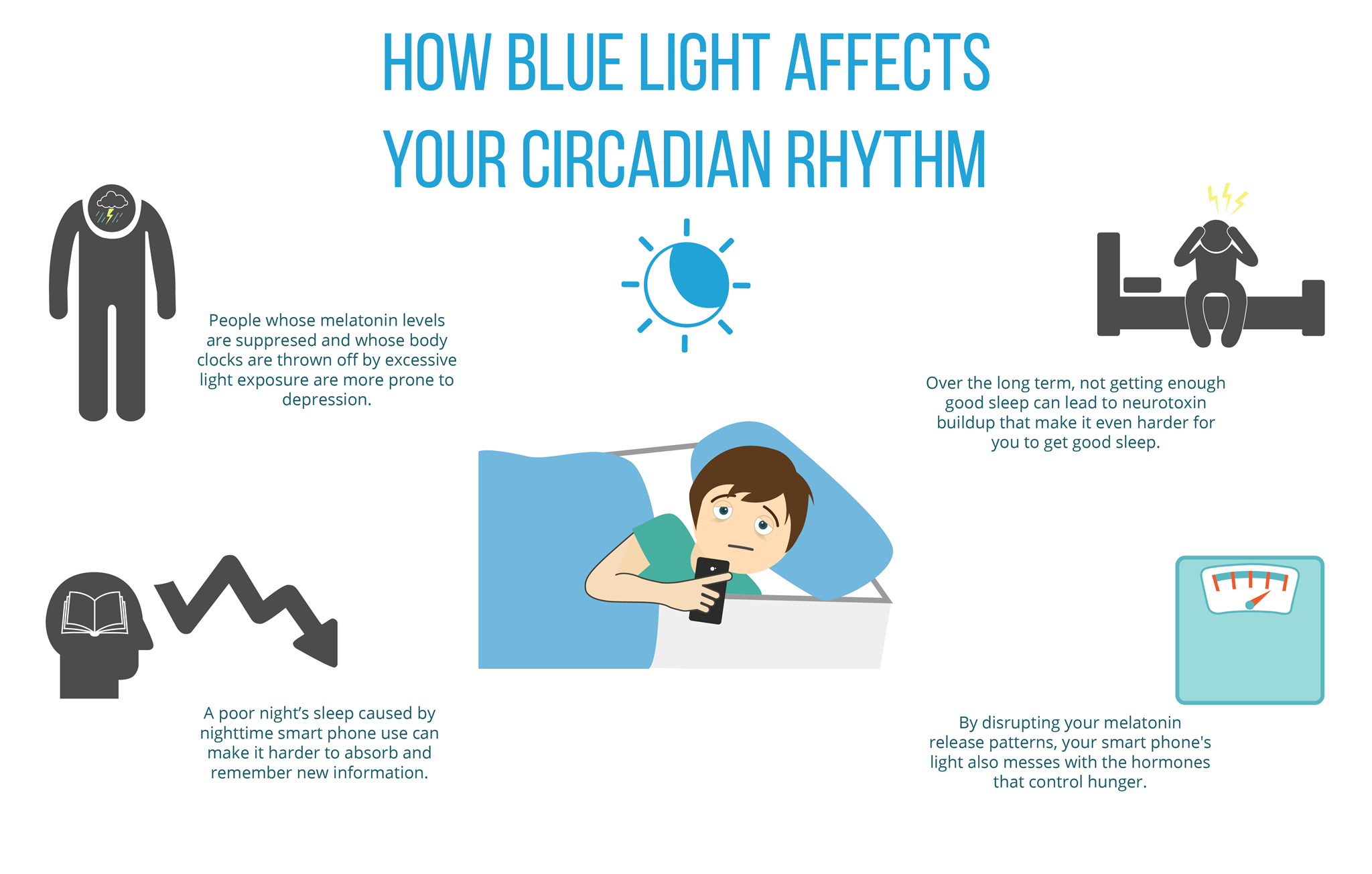
Talieh Ghaneh: Our body is confused—it doesn’t know when it’s day and when it’s night—because during the day we don’t get that much of the intense natural light that you’d get outdoors. And at night, when you’re not supposed to get any blue light, you get a lot of blue light.
When light enters our eyes it travels through two separate pathways. For a long time scientists were aware of one pathway, the visual pathway that connects the retina to the visual cortex and helps us perceive the world around us.
Recently, we’ve learned that light also travels through this new set of photoreceptors called intrinsically photosensitive Retinal Ganglion Cells (ipRGCs) and they contribute mostly to the biological pathway. The biological pathway sends a signal to our master biological clock (a very small area in the hypothalamus) and this clock gets synchronized with the cues it receives from the external environment.
When the retina sends information about the light in the environment to the biological clock, it can trigger melatonin secretion, hormone production, digestion, increased or decreased muscle strength, core body temperature regulation, and immune response—everything is responding to the biological clock. And the whole thing is governed by signals from light in the environment and how it synchronizes with the internal clock.
For millions of years, humans were exposed to a pattern of sunlight in the morning gradually decreasing through to nighttime.
And at night, human beings were not really exposed to high intensity light. Our main source of light in pre-history was the light from the moon, stars and fire.
After 1880 when electric lighting was discovered, as humans we spend more and more time indoors. Today, more than 90% of our time is spent indoors. We spend a lot of time at night at home: watching TV, surfing on our iPads, iPhones, and our computers late at night. And those have a lot of blue light—there’s more energy in the blue part of the spectrum—which our biological system is really sensitive to.
I think it’s really a public health issue. Right now a lot of the policies and the technology are focused on the visual effects of light and not really considering the biological effects of light—because we don’t see it, it’s not tangible. We don’t really know what’s going on and we can’t really quantify this light, so it’s very hard to pinpoint where the problems are. But we are starting to see all these issues. It might be too late when we finally realize what we have done to our bodies.
Language of Light: I have heard some information in the media about the health effects of blue light from electronic devices. Do you think the issue is getting enough publicity?
Talieh Ghaneh: I don’t really think it’s enough. I think receiving proper lighting throughout the day should also be a part of our lifestyle. It’s not just about proper lighting design, it’s also just little things that are important—we need to spend one to two hours in the morning under daylight. If we’re not receiving enough daylight in the morning, we should make sure that in our workspace, in our hospital room, whatever space that we are confined to, we have high intensity, high CCT (correlated color temperature) light sources with high blue content during the day. We need to have that kind of exposure for at least one hour in the morning.
And this is going to help our biological clock to be reset everyday. There are multiple studies that show that effective lighting can really benefit healthcare outcomes. Subsequently reducing the cost of healthcare and perhaps more importantly, saving lives.
At night, if you need to study late or you have to work late, there are tinted goggles with orange or amber-colored hues that you can wear. Apple has added Night Mode to the iPhone which, when activated, removes blue hues from your phone.
Also, we should look to policy. Right now, most commercial and industrial facilities are transitioning from fluorescent to LED. The benefits of smart LED Lighting systems are that we can easily tune the light color temperature, its intensity, and program the system to mimic the spectrum of daylight throughout the day.
And I think this is significant, especially in spaces where lighting is really important—my main research has been in a hospital setting. In a hospital, we know that patients are confined to a particular space due to their physical limitations. They can’t really go out and they are generally not exposed to the outdoors or enough daylight. We are trying to get the same kind of lighting capability from the dynamic light source that LED provides.
In a hospital, you have a very consistent type of lighting throughout the day and night. They turn the light on when the nurse comes in to do checkups. And that’s very uncomfortable for the patient and it also messes up their biological system. And if the patient’s rest and relaxation isn’t activated enough, then they can’t recover fast enough, their medication doesn’t work as well . . . There are multiple studies that show that effective lighting can really benefit healthcare outcomes. It reduces the cost of healthcare. Patients are taking less pain medication when they are exposed to better lighting, the length of stay is shorter, and depression decreases in patients with dementia.
Language of Light: Is that what you would like to see in the future?
Talieh Ghaneh: The process has already started. There are a few hospitals in Europe that are already doing this. Yes, this will be the future of healthcare lighting design—I really believe it. It should be mandatory in hospital settings because it’s really key to the healing process of the patient, as well as the productivity and efficiency of the staff: the nurses, the doctors. If you provide proper lighting in the nurse’s station at night they can be more alert and more productive.
Language of Light: Do you have any other tips for people who are trying to be healthier in the light they are exposed to?
Talieh Ghaneh: Healthy lighting goes hand in hand with healthy darkness. My best advice from what I learned in my research on light and health is that our biological system needs contrast. So it cares about the contrast between the light that you are exposed to during the day and the darkness that you are exposed to during the night. Healthy lighting goes hand in hand with healthy darkness.
Dim the lights in your home as you get closer to bedtime. Two hours before bedtime, eliminate digital screens. And in the day, if you can spend even 15 minutes of your lunchtime outdoors, do it, be exposed to high-level light that can regulate your circadian system, so you can sleep much better at night and be more productive during the day.
Language of Light: That sounds like really great advice. What about for someone who is on a night shift schedule?
Talieh Ghaneh: There’s been a lot of research about people who work the night shift. We’ve learned that it’s possible to shift the phasing of their circadian system.
With a lighting prescription that a light and health specialist can provide, we can change the phase shift of the circadian system so that it is in harmony with a work schedule. The problem is when you have rotating shifts—the rotating shift is worse because you get used to one biological cycle, and then two days after [that] you switch to a day shift and that destroys everything. It’s better to stay on a consistent night shift then switch to a consistent day shift and back if necessary.
For night shift workers, there’s a lot of research on what type of light you should give them. At nighttime our circadian system responds to pulses of light. During the day we need two hours of high intensity blue light (between 1 to 2 hours minimum) to reset our circadian system. At night time we don’t need continuous light, our circadian system responds to cycles, 10 minutes of bright light and then just regular light, and then another 10 minutes [of bright light]—in intervals. So we do four to five intervals of 10-15 minutes of bright, high intensity, high CCT light at night. That works better.
Language of Light: Would the ideal [in the workplace] be to program the system to match daylight?
Talieh Ghaneh: The ideal would be mimicking daylight, that would be the best, healthiest option. What I’m saying is matching the dynamic nature of daylight: going from high color temperature (high blue content) to lower, and in the same way, lowering the intensity gradually as the day progresses.
If you’re doing lighting on a budget, consider skylights in break-rooms. So when people go in the morning to get their coffee or when they go to lunch, for 30 minutes to one hour they are exposed to a lot of high intensity natural blue daylight.
But in order for our biological system to be reset in the morning we need to be getting at least 600 lux at the cornea. The light that reaches our eye—that’s what counts. Sometimes we have a window near our work space, but if you are three, four meters away from the window, the intensity of the light that you get may not be enough.
Language of Light: What is a lighting prescription? Does it come from a lighting designer?
Talieh Ghaneh: Not really, no. Light health is a very new field. There is still a lot that we don’t know. But based on what we do know, we know that light is like a drug to the body. And just like a drug that you need a prescription for, how much you take, when you take it, what dosage, how many times a day, lighting works the same way.
The visual system responds to light in a fraction of a second. But the circadian system is much slower in its response. It works as a cumulative response rather than a simultaneous response that the visual system has. And it cares about the intensity, the timing, the spectrum of the light, and it cares about prior history of exposure.
So for example, if you are exposed to effective light during the day—high intensity blue light—you would be less sensitive to blue light at night. So if you cheat and work on your iPhone for half an hour before bedtime, your circadian clock wouldn’t be as disturbed as if you were not getting proper lighting in the morning.
So a lighting designer or an architect [considering windows or skylight location] designing for, let’s say, a farmer, should consider the farmer’s circadian system responds differently to light than a computer programmer who spends ten hours at the computer.
Language of Light: So you’re saying that a lighting prescription might be something that a lighting designer might take into account when they’re designing light for a specific setting?
Talieh Ghaneh: The amount of light that a young person needs to have their circadian system reset is much lower than the amount of light that an older person needs to get the same effects.
A farmer’s circadian system responds differently to light than a computer programmer who spends ten hours at the computer.
And I know that right now a lot of people who are into lighting research, they do prescriptions for jet lag. So if you’re traveling they tell you exactly [what to do]—[they ask] when you arrive and what time zone you’re in, and they say, “Okay, so when you arrive you go under the sun for one hour and then you come back and then don’t open your curtains or do this.” And so they tell you exactly at what time you need to sleep so you can shift your circadian clock. It helps you to be in harmony with local time much faster.
Language of Light: Have you designed your own life to reflect your research?
Talieh Ghaneh: No. Not yet. [laughing]
I think it takes time, and practice, and good habits. Right now, yes, if I don’t have a deadline, if I don’t have a presentation coming up, I try to eliminate blue light two hours before bedtime and I really see the difference in my sleep patterns. But I am researching all the time so a lot of nights I have to work till 3, 4 [AM]. Right now my lifestyle is not healthy at all. In the morning if I feel sleepy and I didn’t get enough sleep, I try to spend more time outside. I make sure that I am exposed to some sunlight on my drive to work. And I think that helps. I can feel on the days that are cloudy and I don’t get enough sunshine, I am a lot sleepier. And on sunny days I can see the difference.
Language of Light: What do you see for the future of lighting and what would you like to continue to research?
Talieh Ghaneh: I think the future of lighting eventually has to include the effects of light on human health and well-being. Just like LED lighting, at first a lot of people didn’t really buy into it, because you have to spend more money to save just a little bit of money—by changing to an LED or energy-efficient lighting system. But eventually the technology wins and the price points drop down and more people are into energy-efficient lighting.
And for myself, I want to continue my research into the quantification of light for the biological system. The way our circadian system responds to light is multidimensional. We have a lot of lighting systems that quantify light for the visual system. For example, you can say, “100 lux” and you have a sense of how much light it would be on a task. But when you say 200 lux for the circadian system, it can really be nonsense, because we can’t really visualize it or quantify it.
We have to come up with a new matrix to quantify light for the biological system. So we can say, “Okay, this light source provides 50 such-and-such units for the circadian system” and it’s either good or bad. That’s something that I’d like to continue working on.